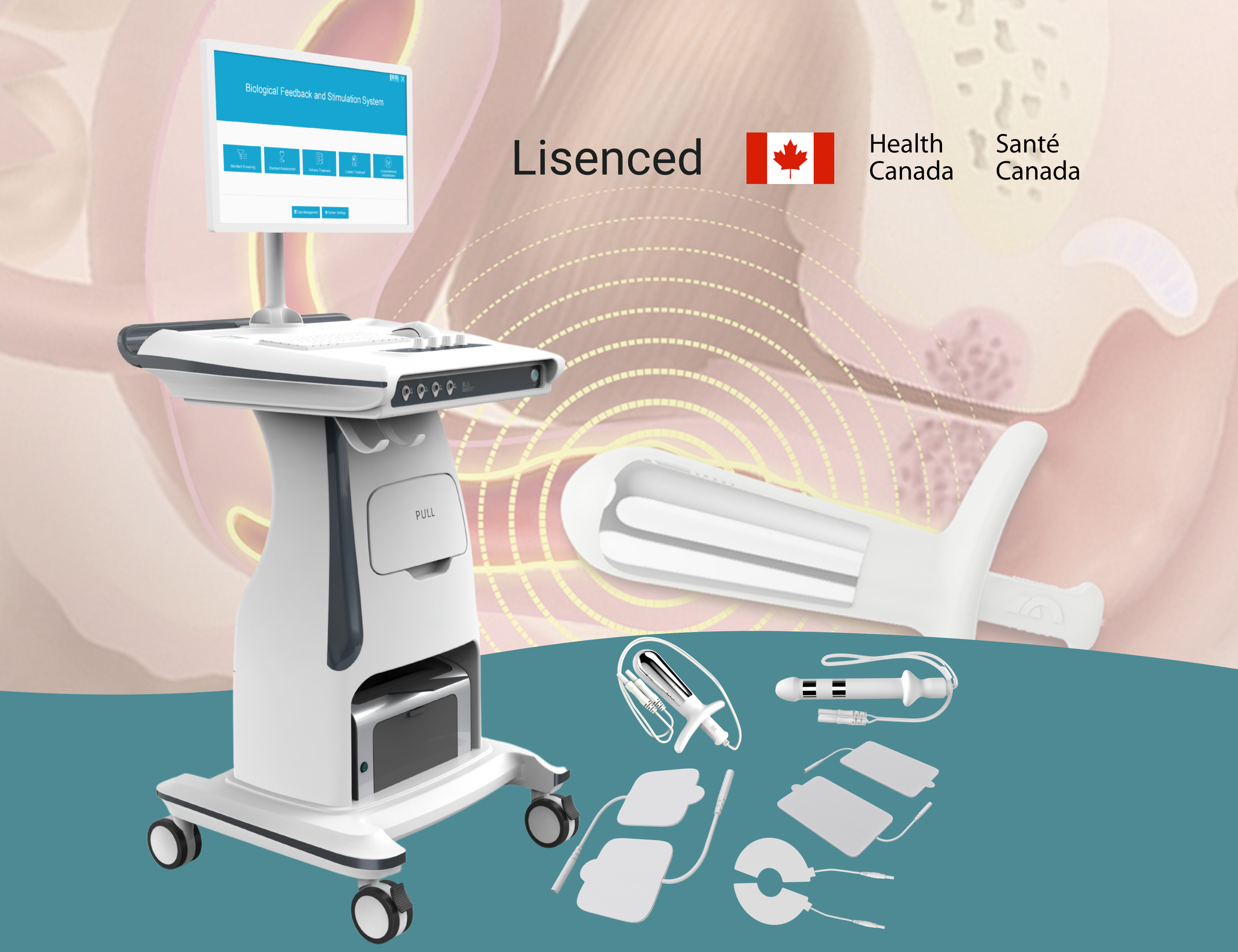
Introduction: Pelvic health physiotherapists strive to provide the best care for women suffering from issues like incontinence, pelvic pain, or postpartum muscle weakness. Traditionally, therapists relied on subjective feedback and manual exams to gauge pelvic floor function. Today, technology is transforming pelvic floor rehabilitation by giving physiotherapists objective data and new treatment modalities. EMG biofeedback and electrical stimulation devices, such as the Medlander B4Plus system, are empowering clinicians to assess muscle performance accurately and enhance therapy outcomes.
Objective Assessment Beyond “Guesswork”
In a pelvic physiotherapy session, being able to measure a patient’s muscle engagement is a game-changer. Biofeedback devices record the electrical activity of pelvic floor contractions, displaying live graphs and numerical values. This means a therapist can immediately see if a patient is activating the correct muscles, and how strongly. It removes the guesswork from Kegel exercises. Using an EMG-based pelvic therapy device, a physiotherapist can conduct standardized evaluations, identify specific muscle weaknesses, and tailor a treatment plan based on real data rather than just symptoms. Patients also gain awareness – they can visualize their pelvic muscle contractions on-screen, which helps them learn to perform exercises more effectively.
Combining Biofeedback with Stimulation
Beyond assessment, modern devices combine EMG biofeedback with electrical muscle stimulation to actively assist in training. The B4Plus system, for example, can prompt patients to contract, and when the patient’s effort reaches a set threshold, the machine delivers a gentle electrical stimulus to augment the contraction. This EMG-triggered stimulation reinforces proper muscle activation patterns. By alternating active patient effort with device-driven stimulation, therapy sessions become more efficient. Research suggests that this combined approach yields superior results: one clinical trial showed that a biofeedback-plus-stimulation protocol achieved a 93.3% overall success rate, compared to 73.3% with a stimulation-alone mode in treating pelvic floor dysfunction. Another study demonstrated significant objective improvements in pelvic floor strength and bladder control when using biofeedback therapy – patients had measurably stronger contractions and fewer leakage episodes after treatment, with urinary leak frequency dropping and pelvic muscle strength scores rising (P<0.01).
Better Outcomes for Patients and Practices
For physiotherapists, embracing EMG biofeedback technology means more effective treatments and happier patients. Women are often amazed to see quantifiable progress in their strength and symptoms over a series of sessions – for instance, seeing their maximum contraction EMG values climb or their urinary leakage incidents fall. This boosts patient motivation and compliance with pelvic floor exercise programs. Clinically, better engagement translates into better outcomes, like higher continence improvement rates and faster recovery times. By offering cutting-edge women’s wellness technology in the clinic, pelvic health specialists can set themselves apart and build a reputation for innovative, evidence-based care. Ultimately, these tools allow physiotherapists to do what they do best – help women regain pelvic health – with greater precision and confidence in the results.
References:
- Tao R. (2024). Biofeedback + stimulation vs. stimulation-alone – 93.33% total effective rate with combined biofeedback & stimulation therapy vs 73.33% with single-mode therapy.
- He X. (2022). Objective improvements after biofeedback training – Significant increase in pelvic muscle strength and reduction in 72-hour leakage frequency (P<0.01) post-treatment.


Partager:
Treating Acne Scars with Fractional CO2 Laser: What Clinicians Should Know
The Role of Cooling Systems in Skin Safety During Laser Treatments