Introduction
Pelvic floor dysfunction is a common chronic issue after childbirth, leading to problems like urinary incontinence, pelvic organ prolapse, and sexual dysfunction. Vaginal delivery can cause more pelvic floor injury than cesarean delivery – studies show that women who deliver vaginally have higher rates of pelvic floor disorders compared to those with C-sections. This makes early rehabilitation crucial, especially for women who delivered vaginally. Pelvic floor physical therapy interventions, including Kegel exercises (the classic pelvic floor exercises for women) and biofeedback training, are essential to restore muscle strength and prevent long-term issues. In fact, research indicates that supervised pelvic floor exercise programs can significantly reduce postpartum incontinence and prolapse risk. Even though this blog focuses on postpartum women, it’s worth noting that pelvic floor exercises for men are also beneficial for conditions like incontinence and should not be overlooked. Here we discuss a study that used surface electromyography (EMG) guidance (the Glazer protocol) to tailor pelvic floor rehab programs for new mothers, and how it improved outcomes across different delivery methods.
Study Overview (Objective & Methodology)
The clinical study by Qiu et al. aimed to evaluate the clinical value of Glazer surface EMG in guiding postpartum pelvic floor muscle rehabilitation under different delivery modes (vaginal delivery, cesarean section, and episiotomy). A total of 180 women at 42 days postpartum were enrolled and split into two groups: observation group (90 women who received EMG-guided pelvic floor rehab) and control group (90 women who received standard pelvic floor rehab without EMG guidance). Within the observation group, patients were further categorized by delivery mode (30 women per subgroup: cesarean, spontaneous vaginal, vaginal with episiotomy). All participants underwent an 8–10 week rehabilitation regimen. The observation group’s therapy was personalized using surface EMG biofeedback – specifically, the pelvic floor EMG biofeedback system was used to assess muscle function and tailor the training intensity. The control group performed routine pelvic floor muscle training (Kegel-type contractions, vaginal weights, and electrical stimulation) without EMG-adjusted feedback. Key outcome measures included the rate of abnormal pelvic floor muscle tension and the incidence of pelvic floor dysfunction symptoms (like urinary incontinence and prolapse) at 42 days and 10 weeks postpartum.
Key Findings (Results & Statistics)
At 6 weeks postpartum (42 days), there was no significant difference between groups in pelvic muscle tension abnormality rates – roughly similar percentages of women in both EMG-guided and standard rehab had low muscle strength at baseline. However, by 10 weeks postpartum, the EMG-guided rehab group showed a dramatically lower rate of abnormal pelvic muscle tension than the control group (significant improvement, P < 0.05). Notably, within the EMG-guided cohort, women who had delivered via cesarean section had better pelvic muscle tone recovery than those who had vaginal deliveries (both with and without episiotomy) – at 10 weeks, the cesarean subgroup had significantly fewer cases of muscle weakness or pelvic floor disorder than the spontaneous vaginal delivery subgroup. Overall, the incidence of pelvic floor dysfunction at 10 weeks was higher in the control group (standard rehab) compared to the EMG biofeedback group, indicating the EMG-tailored training led to better functional outcomes. In the EMG group, only a small fraction of women still had pelvic floor disorder symptoms at 10 weeks postpartum, whereas in the control group more women reported issues like urinary leakage or prolapse symptoms (statistically significant difference, P < 0.05). Importantly, even among the EMG-guided patients, those who had vaginal births (especially unassisted vaginal deliveries) had a higher rate of residual pelvic floor dysfunction than those with cesarean births. This aligns with the general understanding that vaginal delivery imposes greater stress on pelvic tissues, underscoring the need for targeted rehab for these women. The study’s conclusion was clear: using surface EMG biofeedback to guide and evaluate postpartum pelvic floor training has significant benefits. It improves pelvic muscle strength recovery and lowers the occurrence of pelvic floor dysfunction compared to conventional exercise guidance. The authors specifically recommend paying extra attention to women after vaginal delivery, as they may require more intensive rehab to reach the same recovery as their cesarean counterparts.
Clinical Implications and Relevance
For clinicians and pelvic health professionals, these findings highlight the value of integrating biofeedback technology into early postpartum rehabilitation. An EMG-guided program provides real-time feedback on muscle activation and endurance, allowing therapists to personalize Kegel exercise regimens to the patient’s current strength level. In practice, this could mean adjusting the difficulty of pelvic floor exercises for women based on objective EMG readings – essentially, using data to optimize “Kegel workouts” for each patient. The result is more efficient strengthening of the pelvic floor, especially important for women who have weaker muscles after a strenuous vaginal birth. The study also reinforces that delivery mode influences rehab needs. Women after vaginal delivery (particularly with perineal trauma or operative vaginal births) are at higher risk of pelvic floor dysfunction and thus benefit greatly from advanced biofeedback-assisted therapy. By contrast, cesarean mothers in this study had fewer issues by 10 weeks, though they too improved with training. This suggests clinicians should adopt a tailored approach: for high-risk patients (e.g. older first-time mothers or those with difficult vaginal births), incorporate EMG biofeedback and perhaps intensify the rehabilitation program. The goal is not only to treat existing symptoms but also to prevent long-term complications like stress incontinence or prolapse. It’s notable that EMG guidance helped identify subtle deficits in muscle function and track progress. Such objective measures can also motivate patients by showing them improvements in muscle activity over time, potentially increasing adherence to their pelvic floor exercise regimen. In summary, the study confirms that combining traditional pelvic floor physical therapy with modern biofeedback technology leads to superior outcomes – something pelvic health specialists can leverage in postpartum care.
Application and Integration with DioLaz Devices
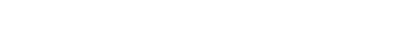
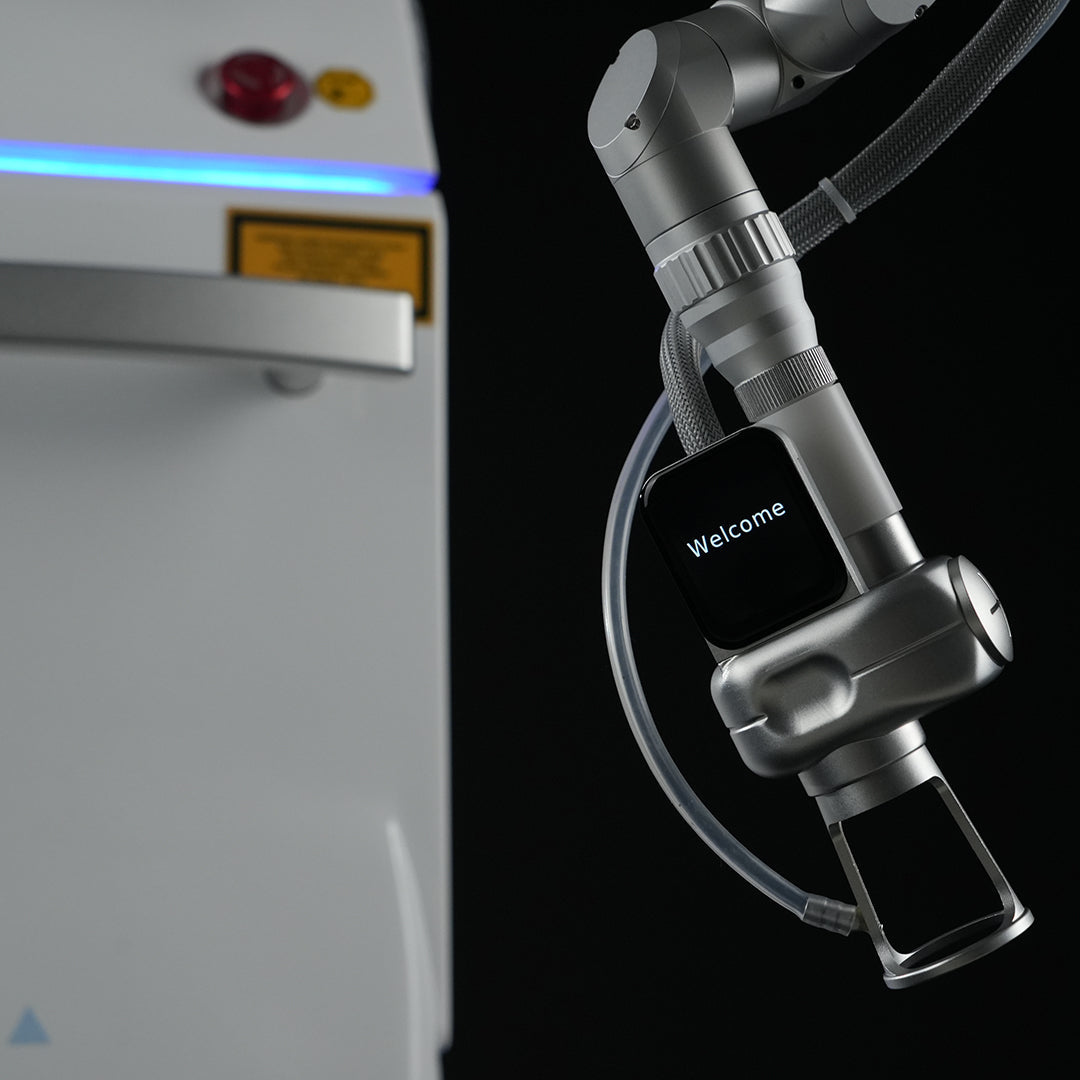
This research directly supports the use of devices like the DioLaz Pelvic Floor Biofeedback and Stimulation System in clinical practice. In fact, the equipment used in the study – the surface EMG biofeedback system – is representative of the advanced technology now available to therapists. DioLaz pelvic rehab systems provide precisely this kind of EMG monitoring and biofeedback training capability. By using vaginal EMG sensors, the system can quantify a patient’s pelvic floor muscle contractions (strength, endurance, and coordination) and display this information in real time. Clinicians can then guide patients through Kegel exercises with visual and auditory feedback, ensuring the correct muscles are engaged – much like the Glazer protocol used in the study. This means that incorporating a DioLaz device into your postpartum rehabilitation program can help replicate the improved outcomes seen in the trial. For example, a therapist could perform an initial EMG assessment at the 6-week postpartum check (similar to the study’s 42-day assessment) to identify any deficits. The device will highlight whether a new mother has poor muscle endurance or low maximal contraction strength. Using those results, the therapist sets up a personalized training plan: perhaps biofeedback sessions three times per week where the mother practices contracting her pelvic floor to hit targets shown on the screen, interspersed with standard pelvic floor exercises at home. Over the next 8–10 weeks, the DioLaz system can track gains in muscle pressure and EMG amplitude, automatically adjusting the difficulty (for instance, increasing the target contraction duration as strength improves). This ensures progressive training – analogous to increasing weights in a gym routine, but here we’re increasing neuromuscular challenge to the pelvic floor. Such biological feedback and stimulation systems not only strengthen muscles but can also improve motor control and coordination, which is critical for functions like continence. Importantly, devices like the DioLaz can store data and generate reports, which help clinicians document improvement in objective terms (e.g. “vaginal resting pressure improved, EMG amplitude during maximal contraction increased by 30%”). These metrics resonate with both medical professionals and patients: they validate the treatment’s effectiveness and can justify continuing therapy or insurance coverage. Furthermore, having a biofeedback and stimulation system in your clinic can attract clients who are seeking the latest, evidence-backed therapies for postpartum recovery. In today’s informed consumer environment, many clinic owners find that offering high-tech pelvic floor rehabilitation (such as EMG-guided pelvic Pilates exercises or stimulation therapy) distinguishes their practice. By referencing studies like this one, you can confidently explain to patients that the integrated approach – exercise plus device – is proven to expedite recovery and prevent issues like incontinence.
Conclusion
In summary, surface EMG–guided pelvic floor rehabilitation significantly enhances postpartum recovery outcomes. The study reviewed demonstrated faster restoration of pelvic muscle strength and reduced pelvic floor disorder rates when EMG biofeedback was used as an adjunct to standard Kegel exercise routines. For pelvic health professionals, this is a compelling case to modernize postpartum therapy protocols. Utilizing advanced biofeedback devices helps ensure that new mothers, especially those who underwent vaginal births, regain pelvic function more completely and quickly. This leads to better long-term continence, pelvic organ support, and sexual health – ultimately improving quality of life. If you’re a clinician or clinic owner, consider integrating the DioLaz Pelvic Floor Biofeedback and Stimulation System into your practice. By doing so, you align your services with cutting-edge research and provide patients with the best tools to succeed in their rehabilitation. The DioLaz Pelvic Floor system offers the same type of EMG feedback utilized in this study, along with gentle electrical stimulation options to further accelerate muscle strengthening. Take action today by exploring our product page for the DioLaz Pelvic Biofeedback and Stimulation System (a technology on which this study was based) – see how it can elevate your pelvic floor therapy offerings and support your patients’ recovery journeys. Empower your clients with measurable progress and help them reclaim confidence in their bodies after childbirth. Together, let’s implement evidence-based solutions that make postpartum pelvic floor rehab more effective than ever.
References:
Baud, D., Sichitiu, J., Lombardi, V., De Rham, M., Meyer, S., & Achtari, C. (2020). Comparison of pelvic floor dysfunction 6 years after uncomplicated vaginal versus elective cesarean deliveries: A cross-sectional study. Scientific Reports, 10(1), 21509. https://doi.org/10.1038/s41598-020-78625-3
Qiu, L. (2020). Guiding and assessing postpartum pelvic floor rehabilitation with Glazer surface EMG for different delivery modes. Journal of Clinical Medicine in Practice, 41(9), 22–24.

Partager:
Healing Diastasis Recti: Pelvic Floor Technology for Core Restoration