Introduction
Preventing pelvic floor disorders is just as important as treating them, especially in the immediate postpartum period. Childbirth (particularly vaginal delivery) can injure pelvic floor muscles to varying degrees, leading to problems such as pelvic organ prolapse or stress urinary incontinence in roughly one-third of women after delivery. Because of these risks, there is growing emphasis on proactive postpartum care – not only instructing new mothers in Kegel exercises and lifestyle adjustments, but also leveraging technology to strengthen the pelvic floor before significant dysfunction sets in. The idea is to intervene early with rehabilitation to prevent pelvic floor dysfunction (PFD) rather than waiting for severe symptoms to arise. In line with this, many modern postpartum programs combine traditional nursing care (education, exercise guidance) with tools like biofeedback or electrical stimulation devices. These devices can enhance muscle activation and help new moms perform pelvic floor exercises correctly. Indeed, a recent systematic review found that pelvic floor muscle training in the first year postpartum can reduce the odds of urinary incontinence by 37% and pelvic organ prolapse by 56% compared to no exercise. This highlights how crucial early interventions are. In this section, we examine a Chinese study that investigated postpartum nursing care plus use of a pelvic floor rehabilitation device versus routine care alone, focusing on high-risk women. The goal was to see if this combined approach yields better pelvic floor muscle recovery and lowers the incidence of PFD in the weeks following childbirth.
Study Overview (Objective & Methodology)
Zeng et al. (2021) carried out a study titled “Effect of postpartum care combined with pelvic floor rehabilitation device on prevention of female pelvic floor dysfunction.” The objective was to determine whether adding device-based pelvic floor therapy to standard postpartum nursing care could improve pelvic muscle recovery and prevent pelvic floor dysfunction in women at high risk for PFD. The study included 80 postpartum women identified as high-risk for pelvic floor dysfunction. (“High-risk” likely means they had risk factors such as multiple vaginal deliveries, forceps/tear, big baby, or maybe obesity, though the criteria were not fully detailed in the snippet beyond being vaginal births.) These 80 women were randomly divided into two equal groups (40 each):
-
Control Group: Received routine postpartum care only. This standard care included postpartum education (teaching mothers about pelvic floor issues and preventive principles) and instructing them in basic pelvic floor muscle exercises (i.e. voluntary contraction of the levator ani, akin to Kegel exercises). Nurses provided guidance on correct technique – e.g. contract the pelvic floor for ~3 seconds, relax for ~4 seconds, do 30 minutes of such exercises twice a day. Importantly, this routine care essentially covered what many hospitals do: education on pelvic floor exercises for women and encouragement to do them regularly at home. No specialized equipment was used for this group.
-
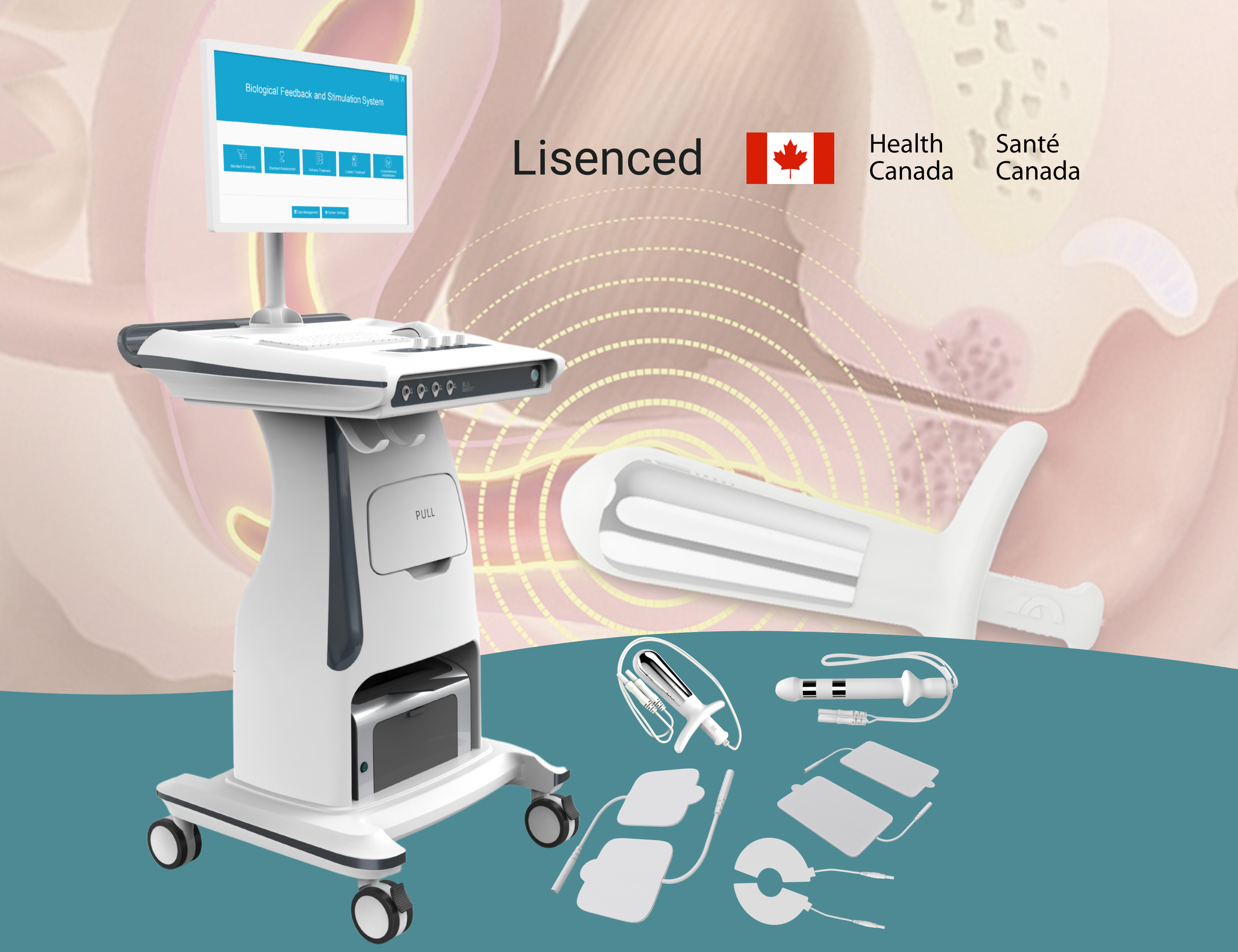
Observation Group: Received the same routine postpartum care plus sessions with a pelvic floor rehabilitation device. Treatment with the device was administered after the mother emptied her bladder and was placed in a lithotomy (supine) position. The vaginal probe was inserted and positioned at the level of the cervix external os. Electrical stimulation parameters were set in a range of 30–80 Hz frequency; the current intensity was titrated up to a level where the patient felt stimulation but no pain (max not exceeding 100 Hz). Four electrode pads were placed on the skin (likely on the lower abdomen or hips) to complete the biofeedback circuit. The device’s regimen was roughly 20–30 minutes per session, 2–3 sessions per week over a 3-week period. Essentially, this group did everything the control did (education + voluntary exercises) and got passive pelvic floor muscle training via the device’s electrical stimulation and biofeedback.
Before the intervention, all women were assessed ~6 weeks postpartum (42 days) to establish baseline pelvic floor status (ensuring no active infection or complications, and all were vaginal deliveries per inclusion). The outcome measures evaluated after 3 weeks of intervention included: 1) Pelvic floor muscle EMG activity – specifically surface electromyography values for fast contractions, sustained contractions, and endurance (also called “resistant contraction”) of the pelvic floor. These reflect how well the muscle fibers can contract quickly, hold a contraction, and resist fatigue. 2) Incidence of pelvic floor dysfunction – defined by occurrence of symptoms or conditions like urinary incontinence, prolapse, etc., checked at the 3-week mark. Essentially, they wanted to see if fewer women developed any PFD symptoms in the device-assisted group versus the standard care group over that short period.
Key Findings (Results & Statistics)
After the 3-week intervention, the differences between the two groups were stark and statistically significant:
-
Pelvic Floor EMG Recovery: The observation group (postpartum care + device) showed much higher pelvic floor muscle EMG values across all measured parameters compared to the control group (care alone). Specifically, the average EMG amplitudes for:
-
Fast contraction (quick squeeze) in the device group was 36.33 ± 1.72 µV, versus only 20.38 ± 2.86 µV in the control.
-
Continuous contraction (sustained hold) was 33.41 ± 2.16 µV with the device, compared to 17.02 ± 3.28 µV without.
-
Endurance contraction (resisting fatigue) reached 32.33 ± 2.24 µV in the device group, versus 12.94 ± 2.91 µV in controls.
These are large differences – roughly the device group had nearly double (or more) the EMG amplitude of the control group on each measure. All differences were highly significant (P = 0.0000 for each, essentially P<0.001). This indicates a dramatically better restoration of muscle function when the pelvic floor rehab device was used alongside exercises. In practical terms, women who got the device-assisted therapy could generate stronger and more enduring pelvic floor contractions by the end of 3 weeks, compared to those who only did self-exercises. The EMG data objectively confirm that their muscles were more responsive and capable.
-
-
Pelvic Floor Dysfunction Incidence: In the control group (just standard care), a certain percentage of women developed pelvic floor dysfunction symptoms within those first postpartum weeks (the exact number isn’t given in the snippet, but typical issues might be mild urinary leakage or feeling of prolapse). In contrast, the device group had a significantly lower incidence of pelvic floor dysfunction after 3 weeks. The text states with P<0.05, meaning fewer women in the observation group experienced any pelvic floor disorder compared to controls. Although exact percentages aren’t quoted, we can infer that the combination of nursing care + device prevented some cases that would have occurred with care alone. Essentially, by week 3 postpartum, the device group likely had notably fewer reports of stress incontinence episodes, less pelvic organ descent on exam, or other dysfunction markers relative to the control group.
These findings led to the conclusion that postpartum care combined with a pelvic floor rehab device effectively improves pelvic floor muscle electrical activity and reduces the incidence of pelvic floor dysfunction in high-risk women. In short, the strategy of blending hands-on nursing (education + basic exercise) with technology-assisted exercise (biofeedback & stimulation) was proven superior to just standard advice and Kegels in this immediate postpartum timeframe.
Clinical Implications and Relevance
This study has important implications for both hospital postpartum care protocols and outpatient pelvic therapy programs. First, it validates the approach of early, preventive intervention for pelvic floor health. Traditionally, many women are simply told to do Kegels after birth and only seek help if problems arise. This research suggests we should flip that script: actively provide structured pelvic floor rehab right after delivery (in the first 6–8 weeks) to ward off dysfunction before it becomes harder to reverse. For obstetric units and postpartum nurses, this might mean incorporating a session of pelvic floor muscle activation (using a device or at least teaching aids) during the hospital stay or shortly after. The dramatic EMG improvements in just 3 weeks show that muscles respond quickly to targeted training, so initiating it early can harness the body’s postpartum healing window when muscle plasticity is high.
Second, the results highlight that biofeedback and stimulation devices can markedly amplify the effectiveness of pelvic floor exercises. Many new moms struggle to perform Kegels correctly – some cannot feel which muscles to contract, and others might inadvertently use abdominal or gluteal muscles instead. The device provides an immediate assist by electrically stimulating the pelvic floor to contract and by giving feedback signals. This not only ensures the right muscles are engaged, but likely also accelerates muscle fiber recruitment and strength gains, as evidenced by the nearly doubled EMG readings vs. doing exercises without device. Clinically, this suggests that pelvic health therapists and postnatal fitness specialists should consider adding a biofeedback device session to postpartum check-ups, particularly for those at higher risk (e.g., women with pelvic floor trauma, large babies, or multiple births). It’s akin to jump-starting the muscle recovery process.
Another implication is in preventive strategy for pelvic floor dysfunction. The fact that fewer women in the device group developed PFD symptoms within a month postpartum is notable. It supports the notion that “an ounce of prevention is worth a pound of cure.” If we can prevent even mild cases of incontinence or prolapse early on, we may reduce the need for more intensive therapy or surgery later. For patients, this is a compelling message: engaging in a bit more guided therapy now can spare you significant inconvenience or procedures down the line. This could influence how postpartum care is marketed – not just as recovery, but as prevention of future problems like urine leaks when you sneeze or the need for pessaries/surgeries in midlife.
Additionally, the study underscores the synergy of nursing care and technology. The routine care in this study wasn’t trivial – it involved proper patient education, reassurance, and encouragement to do exercises, which remain fundamental. The device doesn’t replace that; it augments it. Therefore, clinical practice should ensure that any technological intervention (e.g., bringing a mom in for device sessions) is coupled with thorough instruction on lifestyle, posture (perhaps teaching pelvic tilt exercises to improve core support), and self-care. For example, nurses can teach about avoiding heavy lifting early on, doing gentle pelvic floor exercises for women during daily activities (like “Kegels at red lights” technique), and even pelvic floor-friendly Pilates moves for overall core strength. Then, adding weekly device sessions can greatly enhance those efforts.
From a healthcare system perspective, one might ask: is it feasible to implement device therapy for all high-risk postpartum women? If not in every case, this study helps identify a subset who would benefit most: those with risk factors (which could include older age, multiple gestation, long pushing stage, forceps delivery, etc.). For them, scheduling a series of pelvic floor rehab appointments soon after birth could be justified as a standard of care. The outcome improvements could potentially reduce postpartum return visits for issues or improve patient satisfaction scores regarding postpartum recovery.
Application and Integration with DioLaz Pelvic Floor Health System
The device used in this study is one of the products in the category of pelvic floor biofeedback electrical stimulators, and it closely mirrors the capabilities of the DioLaz Pelvic Floor Biofeedback and Stimulation Systems. How can you integrate this into your practice or facility? If you are a hospital-based physiotherapist or nurse, you could set up a postpartum pelvic floor rehabilitation program where before discharge (or at the first postnatal visit) you identify high-risk mothers and schedule them for device-assisted sessions. The DioLaz system is portable and user-friendly, making it feasible to deliver a 20-minute session in a clinic room. As in the study protocol, you would ensure the patient has emptied her bladder and is in a comfortable position, then insert the vaginal probe (with proper consent and explanation). The device’s settings can be adjusted to the patient’s comfort – starting perhaps around 30 Hz and gently increasing until she feels a strong but not painful contraction. The system provides visual biofeedback (maybe a bar or graph moving with muscle contractions), which can be incredibly motivational. The mother can see, for instance, how high the bar goes when the stimulation triggers a contraction and when she adds her own effort to it. Over a few sessions, she’ll likely see that she can achieve a higher contraction on her own as the muscles strengthen (which aligns with the EMG improvements seen in the study).
For outpatient pelvic health clinics, offering a “postpartum prevention package” using the DioLaz Pelvic Rehabilitation device could set your clinic apart. You can advertise that this program pairs one-on-one guided exercise (ensuring correct technique – no cheating with other muscles) with state-of-the-art biofeedback stimulation proven to accelerate recovery. Educate potential clients that such a program not only helps them heal but actively prevents issues like incontinence that often show up months or years later if not addressed. The product pages for the DioLaz Pelvic Floor Biofeedback System contain specifics about protocols for postpartum use, and you can adapt those to individual patient needs. For instance, younger, first-time moms with minimal trauma might do well with just a couple of sessions and home guidance, whereas those with more risk factors could come in twice weekly for a month. The device’s flexibility allows all that.
Additionally, the DioLaz Pelvic Floor Health system often come with preset modes targeting different aspects (e.g., one mode might focus on endurance, another on quick flicks). You can utilize those exactly as the study did – possibly starting with a mode that wakes up slow fibers (lower frequency, longer pulse, to improve baseline tone and endurance), then gradually incorporate higher-frequency contractions to train the fast fibers for quick responses (important for preventing stress leaks during sudden exertion). This multimodal approach was likely part of why the observation group’s EMG improved so uniformly across parameters.
A practical tip: incorporate this device therapy into the context of holistic care. For example, many postpartum women come to clinics for breastfeeding support, C-section wound checks, or baby’s check-ups. Co-locating pelvic floor rehab with those visits can be convenient. With the efficient 20–30 minute session that DioLaz devices offer, a mom could potentially have a pelvic floor session while waiting for another appointment. Consider collaborating with obstetricians or midwives – they identify the need, and your clinic provides the solution.
Conclusion
The evidence is clear that combining proactive nursing care with pelvic floor biofeedback/stimulation devices soon after childbirth yields superior outcomes for pelvic floor health. By boosting muscle strength and preventing early signs of dysfunction, this combined approach can set new mothers on a path of confidence and comfort. For healthcare professionals and clinic owners, the message is to embrace innovation in postpartum care: don’t rely solely on pamphlets and verbal instructions – integrate technology that can dramatically improve how well and how fast your patients recover. The DioLaz Pelvic Floor Biofeedback and Stimulation System is precisely such a technology, designed to bring hospital-grade pelvic rehab to your practice in a user-friendly way. If you’re interested in elevating your postpartum services, we invite you to explore our DioLaz product line – specifically the DioLaz Pelvic Biological Feedback and Stimulation System – which is featured on our website. There, you can find detailed information and videos about how it works and the results it can achieve. This is the same class of device that helped women in the study regain nearly double the muscle strength in just weeks. Imagine the reputation your practice could build by offering that level of care! We encourage you to contact us for a demo or consultation on implementing a postpartum pelvic floor program. By taking action now, you’ll not only be supporting sales of a proven system but, more importantly, fostering better health outcomes for countless women. Incontinence and prolapse are not inevitable consequences of motherhood – with the right interventions, they can be prevented. Let’s work together to make advanced postpartum rehabilitation a standard, so new moms can focus on their babies and not on rushing to the bathroom or dealing with discomfort. Invest in prevention, equip your clinic with DioLaz, and become a leader in pelvic health for women in your community.
References
Beamish, N. F., Davenport, M. H., Ali, M. U., Gervais, M. J., Sjwed, T. N., Bains, G., Sivak, A., Deering, R. E., & Ruchat, S.-M. (2025). Impact of postpartum exercise on pelvic floor disorders and diastasis recti abdominis: A systematic review and meta-analysis. British Journal of Sports Medicine, 59(8), 562–575. https://doi.org/10.1136/bjsports-2024-108619
Zeng, X., Ye, F., Luo, F., Li, S., & Li, L. (2021). Preventive effect of postpartum care combined with pelvic floor rehabilitation device on female pelvic floor dysfunction. Medical Equipment, 34(24), 130–131.


Share:
Anti-Aging Benefits of GHK-Cu – How Copper Peptides Rejuvenate Skin