Introduction
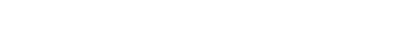
Lip-tie and tongue-tie (ankyloglossia) are conditions where restrictive frenum attachments limit the normal mobility of the lip or tongue. These tethered oral tissues can lead to breastfeeding difficulties in infants, speech impediments, oral hygiene challenges, or other functional issues in children and adults. Traditionally, frenectomy (removal or release of the frenum) has been performed with scalpels or scissors, often requiring sutures and having notable postoperative discomfort. However, the advent of laser dentistry – especially the use of CO2 lasers – has transformed the management of lip and tongue ties. The DioLaz Fractional CO2 Laser is one such advanced tool that allows practitioners to perform frenectomies in a quick, precise, and virtually bloodless manner. In this article, we examine the use of CO2 laser frenectomy in both pediatric and adult patients, highlighting clinical outcomes, procedural efficiency, patient comfort, and how it compares to conventional methods. An evidence-based perspective is provided through international studies to demonstrate the advantages of laser frenectomy and how the features of the DioLaz CO2 laser align with modern clinical needs.
Precision and Efficiency of CO2 Laser Frenectomy
CO2 lasers offer unparalleled precision in soft-tissue surgery, which is particularly beneficial for frenectomy procedures. The laser’s focused beam cleanly incises the frenum tissue while simultaneously coagulating blood vessels. This results in an exceptionally dry surgical field – a stark contrast to the bleeding often encountered with scalpel frenectomies. Clinicians report that using a CO2 laser yields a “dry and bloodless field during operation”, greatly facilitating visualization and accuracy. The efficient cutting ability of the laser also shortens the procedure time. A 2021 systematic review comparing laser versus conventional frenectomy found that laser surgeries had significantly shorter operative times on average. Without the need to stop for bleeding control or suture placement, a typical laser frenectomy can often be completed in minutes. This efficiency is valuable, especially when treating infants or uncooperative children – the shorter the procedure, the less stress for both patient and clinician.
Importantly, the DioLaz CO2 Laser system provides both continuous and fractional modes, giving the practitioner control over the laser’s intensity and pattern. In surgical mode, the DioLaz can make a full-thickness incision through the frenulum with pinpoint accuracy, releasing the tie completely. The laser’s energy is highly absorbed by the water in mucosal tissues, meaning it vaporizes the target tissue with minimal damage to adjacent areas. This precision reduces the risk of inadvertent injury to nearby structures (such as salivary duct openings or muscle fibers) compared to a scalpel. Additionally, the coagulative properties of the CO2 laser seal small blood vessels and lymphatics immediately, which has two key effects: nearly no bleeding and less postoperative swelling. Because of this, no sutures are usually required after a CO2 laser frenectomy – the wound edges are effectively cauterized and stabilized by a thin coagulum. Multiple studies have documented that in laser frenectomy cases, 0% of patients needed suturing, whereas essentially all scalpel cases did require sutures. The elimination of sutures not only saves time but also spares the patient the foreign-body irritation and an additional appointment for suture removal.
Another aspect of efficiency is anesthesia. With conventional frenectomy, local anesthesia via infiltration is standard (and young children may even need general anesthesia for cooperation). CO2 laser frenectomy, however, often demands less anesthetic intervention. The laser’s ability to work quickly and its partial analgesic effect (from sealing nerve endings) mean that some cases can be done with only topical anesthetic or minimal infiltration. In fact, research indicates significantly fewer patients require injectable local anesthesia when undergoing laser frenectomy compared to scalpel surgery. One report noted that all scalpel frenectomies in a series used infiltrative anesthesia, but only 40% of the laser frenectomies needed injections (the rest managed with topical or no anesthetic). This is a major advantage in treating infants, where avoiding injections reduces trauma, and in adults who may have medical contraindications or anxiety about needles. The DioLaz laser allows for such delicate control that, in infants, many practitioners perform a quick “snip” of a tongue-tie with just a drop of topical anesthetic, completing the entire release in seconds. Overall, the precision and efficiency of the CO2 laser approach streamline the frenectomy procedure considerably, aligning with a dental practice’s goal to deliver effective treatment with minimal intervention.
Patient Comfort and Healing: Laser vs Traditional Frenectomy
Perhaps the most compelling advantages of CO2 laser frenectomy lie in patient experience and postoperative outcomes. Laser frenectomies are widely reported to be less painful and easier in recovery than conventional techniques. The immediate sealing of nerve endings by the laser’s heat is thought to reduce intra- and post-operative pain. Clinical studies provide evidence supporting this: a systematic review of frenectomy outcomes found that laser-treated patients experienced significantly less postoperative pain and required fewer painkillers than those who had scalpel frenectomies. For example, on the day of surgery and the first few days after, pain scores were lower in the laser group in the majority of reviewed studies, sometimes markedly so. Many patients describe only mild soreness or a “burning” feeling for a short period, which is easily managed with over-the-counter analgesics if needed. In some cases, especially with infants, caregivers report that the baby seems comfortable enough to feed almost immediately after the procedure when a laser is used.
Postoperative swelling and inflammation are also reduced with laser frenectomy. The CO2 laser’s photothermal action causes a protein coagulum that acts like a natural wound dressing, preventing excessive edema. One clinical case series noted no postoperative swelling, pain, or discomfort following CO2 laser tongue-tie release, with normal healing observed. This is in stark contrast to the swelling and ulceration that can occur after a scissor/snip frenotomy. The gentler healing process with lasers often means infants and children have less difficulty feeding or speaking during recovery. In terms of wound healing, although laser wounds heal by secondary intention, the outcomes are excellent. The healing tends to be quick and unproblematic, with a soft tissue fill that occurs without intervention. In fact, some research observed that laser frenectomy sites healed with no scarring and a normal frenulum morphology over time, whereas scalpel sites can sometimes heal with fibrous scar tissue or reattachment if not properly managed.
It’s worth noting that there is some nuanced evidence regarding pain: a recent randomized trial in 2–6-year-old children reported that CO2 laser cases had slightly higher immediate postoperative pain scores than scalpel cases, yet by one month post-surgery the laser group showed greater improvements and higher parent satisfaction. The initially higher pain in that study could be due to the laser char or open wound (versus a sutured scalpel wound), but despite that, the overall outcomes favored the laser in terms of function and satisfaction at follow-up. This underscores that proper analgesic care (e.g. topical gels or analgesics) in the first days can easily manage any laser-associated discomfort, and the longer-term benefits – like better tongue/lip mobility and no scar tethering – become more apparent with time.
Another advantage of CO2 laser frenectomy is reduced risk of complications. Bleeding is minimal, so postoperative hemorrhage is rare to nonexistent (especially critical in infants, where even small bleeding can be dangerous). Infection risk is low as the laser sterilizes the wound. There is also evidence that laser frenectomies have a lower chance of frenum reattachment. Because the laser effectively vaporizes the collagen fibers and epithelial lining in the frenum area, it may delay re-epithelialization in a way that discourages reconnection of the tissues (when combined with post-op stretching exercises). Parents often report easier feeding or improved speech quite soon after a laser procedure. For infants, successful tongue-tie release with a CO2 laser can lead to almost immediate improvements in latch and nursing comfort, as noted in various pediatric case reports. For older children and adults, benefits include improved articulation of speech sounds (for tongue-tie) and reduced gaps or periodontal stress between teeth (for lip-tie).
From the patient’s perspective, the laser procedure is generally less frightening as well. There is no scalpel or scissors “snip” – instead, the experience is of a quick light application often described as feeling warm. The lack of needles (in many cases) and the absence of sutures make the process feel less like surgery. This psychological comfort should not be underestimated, especially in pediatric dentistry. In fact, in surveys, more patients (and parents) prefer the laser technique if they’ve experienced both methods. The high satisfaction scores stem from the combination of a simpler procedure, smoother recovery, and excellent clinical results. Thus, CO2 laser frenectomy not only addresses the anatomical problem effectively but does so in a way that maximizes patient (and parent) comfort and confidence.
Clinical Outcomes in Pediatric vs. Adult Patients
Infants and Children: In infants, a tight lingual frenulum can severely hinder breastfeeding, causing maternal pain and poor weight gain for the baby. CO2 laser frenectomy has become a popular approach for releasing tongue-ties in newborns and infants because it is extremely fast and minimally invasive. Many infant frenectomies with a CO2 laser can be performed in an office setting with just a topical anesthetic or a quick swaddle, taking under 30 seconds of laser time. The results are often dramatic – mothers frequently report immediate improvement in latch and feeding within hours of the procedure. A study focusing on early laser frenectomy for infants noted highly satisfactory results, calling the treatment “quick” and beneficial in preventing breastfeeding problems. The lack of bleeding is especially important in such young patients; with DioLaz, the clinician can precisely release the tie without any significant blood loss, and the baby can return to nursing right away without the worry of a mouthful of blood. Post-procedure care for infants typically involves some simple tongue stretching exercises and feeding on demand – no dressings or sutures needed. Because the CO2 laser frenectomy is so tolerable, it also reduces the need for general anesthesia in older pediatric cases; many tongue-tied toddlers and children who might otherwise need a hospital visit for a frenectomy under GA can instead have it done awake in the clinic with the laser, avoiding the risks and costs of anesthesia.
For lip-ties in infants (which can affect how the upper lip flanges during nursing or lead to a gap between the front teeth as they grow), the CO2 laser is equally useful. A quick laser lip frenectomy can help improve an infant’s latch seal or later facilitate orthodontic closure of a diastema. Pediatric dentists and oral surgeons have reported that using a CO2 laser on these delicate labial tissues results in minimal fuss from the baby, rapid healing, and no scarring that would impede lip movement. Parents appreciate the simplicity – often describing the laser procedure as appearing almost “bloodless and painless” for their child. Follow-up exams usually show excellent healing in a week or two, with the frenulum effectively released.
Adults: While much public attention is on infants, adults also benefit from laser frenectomy. Some adults have enduring tongue-tie issues that affect speech (for instance, difficulty rolling an “R” sound or limited tongue reach affecting oral hygiene). Others might have a prominent lip frenum causing gum recession or interfering with denture fit. In adults, CO2 laser frenectomy under local anesthesia is a straightforward procedure that can significantly improve oral function and comfort. The healing in adults is equally as good as in younger patients. Adults typically report that the procedure was far less painful than they expected – many feel only mild soreness for a day or two. Because no sutures are placed, patients experience less irritation and can perform tongue movements exercises sooner to maximize the new range of motion. In terms of outcomes, adults often notice improved speech clarity or easier oral hygiene (tongue can reach all areas of mouth). For a lip-tie, an adult patient might see that the gap between teeth is more likely to stay closed after orthodontic treatment, or if wearing a denture, the denture now sits better without the frenum pulling it. The laser’s precise cutting ensures that only the necessary tissue is removed, preserving esthetics (important for a lip frenectomy in the smile zone). A conventional scalpel technique in an adult would require an incision and stitches that might leave a visible scar or cause more post-op discomfort, whereas the laser site heals with minimal trace.
Notably, adult frenectomies with lasers have a very low complication rate. A 2018 study (Uraz et al.) cited in reviews found no postoperative bleeding in either group, but laser patients had less pain and no need for analgesics, and only the scalpel group had a case of postoperative hemorrhage. Additionally, two cases of minor superficial bone exposure were noted in laser groups in one study, but these healed without issue. Overall, complications are rare and typically minor. The high success and low morbidity have made CO2 laser frenectomy a preferred method for practitioners who have access to the technology.
Comparison with Traditional Methods
When directly comparing CO2 laser frenectomy to traditional scalpel or scissor techniques, the consensus in the literature is that lasers offer equal if not superior outcomes in most metrics. According to a systematic review of several clinical studies (375 patients in total), laser frenectomies consistently achieved better perioperative results: shorter surgery duration, no need for sutures, less intraoperative bleeding, and reduced postoperative pain and functional limitations. Patients who had laser surgery could often eat and speak more comfortably in the first week compared to those who had conventional surgery, who experienced more difficulty due to pain or the presence of sutures. The only category where scalpel sometimes held a slight edge was initial wound closure – a sutured scalpel wound might appear “healed” faster in terms of epithelial cover. However, this does not necessarily equate to better functional healing, and some studies even note that final healing and scar formation tend to be better in laser cases (scalpel can sometimes heal with dense scar tissue).
Importantly, patient satisfaction heavily favors the laser. In studies where patients experienced both methods (for example, a diastema patient who had one method and later another, or trials where groups were surveyed), significantly more patients preferred the laser technique and said they would recommend it. This is a powerful indicator for dental practices when deciding on treatment modalities – a happier patient is the best referral source. The DioLaz Fractional CO2 Laser, with its modern ergonomic design and adjustable settings, allows clinicians to perform these frenectomies with consistency and confidence, ensuring that the clinical advantages documented in research translate into real-world practice.
In summary, CO2 laser frenectomy offers a combination of precision, speed, comfort, and excellent outcomes that surpass traditional frenectomy methods on many fronts. Whether dealing with a newborn struggling to feed or an adult seeking to improve oral function, the laser approach addresses the core issue effectively while minimizing collateral trauma. By adopting CO2 laser technology like the DioLaz system, dental professionals can elevate the standard of care for lip-tie and tongue-tie releases – providing patients of all ages a better experience and optimal results backed by evidence-based success.
Conclusion
The use of CO2 lasers for lip and tongue tie releases represents a significant advancement in minor oral surgery. Both clinical evidence and practical experience underscore that laser frenectomy (frenotomy) is a highly efficient, patient-friendly alternative to conventional techniques. The key benefits – minimal bleeding, no sutures, reduced pain, and rapid healing – directly address the main drawbacks of scalpel frenectomy, leading to improved clinical outcomes and patient satisfaction. For pediatric patients, CO2 laser treatment can be life-changing, enabling infants to feed effectively and children to speak properly with minimal intervention. For adult patients, it offers a quick in-office solution to issues that might otherwise require more invasive surgery. The DioLaz Fractional CO2 Laser exemplifies the technology that makes these benefits possible: its surgical precision and dual fractional capability allow dentists to tailor the treatment to each patient’s needs, ensuring a gentle yet thorough frenulum release. In comparing with traditional methods, CO2 lasers come out on top in virtually every category of perioperative outcome, as confirmed by systematic reviews and RCTs. By integrating CO2 laser frenectomy into practice, clinicians can confidently provide a procedure that is evidence-based and widely regarded as the gold standard for managing lip-ties and tongue-ties. Ultimately, this translates into better care for patients – from infants gaining the ability to nurse comfortably to adults finding relief from long-standing oral restrictions – all achieved with the efficiency and excellence that modern laser dentistry delivers.
References
Chiniforush N. et al. (2014). Treatment of Ankyloglossia with Carbon Dioxide Laser in a Pediatric Patient – Case Report. J. Lasers Med. Sci., 5(1): 42–46. PMID: 25606324
Lebret C. et al. (2021). Perioperative outcomes of frenectomy using laser versus conventional surgery: a systematic review. J. Oral Med. Oral Surg., 27(3): 36. DOI: 10.1051/mbcb/2021010
Pardell D. et al. (2020). Infant CO2 Laser Frenectomy Outcomes: Parental Perceptions and Feeding Improvements. Photobiomodul. Photomed. Laser Surg., 38(12): 706–713. DOI: 10.1089/photob.2020.4912
Haytac M.C. & Ozcelik O. (2006). Evaluation of patient perceptions after frenectomy operations: a comparison of diode laser and scalpel techniques. J. Periodontol., 77(11): 1815–1819. DOI: 10.1902/jop.2006.060043
Ghini C. et al. (2018). Laser vs Conventional Lingual Frenectomy in Children: A Retrospective Comparative Study. European J. Paediatric Dent., 19(4): 324–328. DOI: 10.23804/ejpd.2018.19.04.13

Share:
Fractional CO2 Lasers in Dentistry: Versatile Applications and Clinical