Introduction
Laser technology has revolutionized dental practice, offering clinicians new levels of precision and patient comfort. The DioLaz Fractional CO2 Laser, an advanced dental laser with dual fractional and surgical modes, exemplifies this innovation. It enables both targeted cutting (surgical mode) and fractional phototherapy, making it a versatile tool for various soft-tissue procedures. This article explores the broad range of dental applications for fractional CO2 lasers – from routine gum surgeries to aesthetic treatments – and highlights evidence-based clinical advantages such as reduced bleeding, greater precision, faster healing, and improved patient comfort. The aim is to provide dental professionals an academic-style overview of how DioLaz Fractional CO2 lasers can enhance clinical outcomes across multiple disciplines of dentistry.
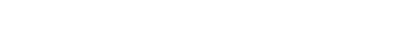
CO2 Laser Precision and Hemostasis in Soft-Tissue Surgery
One of the foremost benefits of CO2 lasers is their exceptional precision and hemostatic capability in soft-tissue surgery. CO2 laser energy (wavelength ~10,600 nm) is highly absorbed by water-rich oral tissues, allowing it to vaporize soft tissue with minimal depth of penetration and collateral damage. As a result, incisions made with a CO2 laser are extremely clean and largely bloodless. Studies have confirmed that lasers – particularly CO2 and certain diode wavelengths – provide superior hemostasis compared to scalpels. The thermal effect of the CO2 beam coagulates small blood vessels as it cuts, creating a dry surgical field with little to no bleeding. This can obviate the need for cumbersome periodontal packing or frequent suction, improving visibility and precision during procedures. Moreover, laser incisions typically do not require suturing because the laser’s coagulation seals the wound margins. The DioLaz laser’s surgical mode leverages these properties, enabling dentists to perform scalpel-free excisions with excellent control and minimal bleeding.
Clinical Benefits for Patients: The precise, thermocoagulative action of the CO2 laser translates to tangible patient benefits. Laser incisions induce less mechanical trauma and immediately seal lymphatic and nerve endings, which leads to reduced postoperative pain, swelling, and inflammation. A recent systematic review of laser gingivectomy procedures found that laser-treated patients consistently reported less post-operative pain and required fewer analgesics compared to those treated with conventional surgery. Additionally, the inherent sterilization effect of laser ablation (due to high temperature) helps lower the risk of infection and bacteremia in the surgical area. By providing clean cuts and disinfecting the tissue simultaneously, CO2 lasers promote favorable healing conditions. Clinical evidence shows that soft-tissue wounds from CO2 lasers heal with minimal scarring and excellent functional results, often via secondary intention but with healthy epithelialization within days. In one study on gingival depigmentation, patients treated with a CO2 laser experienced very mild pain and achieved 100% complete epithelial healing of the gingiva by one week post-op. These outcomes underscore how fractional CO2 laser technology enhances patient comfort and speeds recovery.
Versatile Applications of Fractional CO2 Lasers in Dentistry
Fractional CO2 lasers have a wide array of uses in everyday dental practice. The DioLaz system’s dual capabilities (fractional and surgical modes) mean it can be adapted for everything from surgical incisions to superficial tissue therapy. Key dental applications include:
-
Gingivectomy and Gingival Contouring: CO2 lasers are highly effective for gingivectomy procedures to correct gummy smiles, remove hyperplastic tissue, or reshape gingival margins. Laser gingivectomy allows precise removal of excess gum tissue with minimal bleeding. Studies show laser-assisted gingivectomy produces stable gingival margins and aesthetic outcomes comparable to scalpel surgery, with the added advantages of less intraoperative bleeding and reduced postoperative discomfort. Because the laser cauterizes as it cuts, clinicians can often perform gingivectomies without placing periodontal dressings, improving patient comfort. Fractional CO2 mode can also be used for gingival soft-tissue resurfacing, helping to even out textures or stimulate healing in periodontal therapy.
-
Operculectomy and Tooth Exposure: Removal of inflamed opercula (tissue flaps over erupting molars or impacted teeth) is simplified with a CO2 laser. Laser operculectomy is quick, precise, and virtually painless. In an orthodontic context, lasers are used to expose impacted teeth (such as palatally impacted canines) to aid eruption. Research has demonstrated that patients treated with laser operculectomy report significantly less postoperative pain and swelling than those treated with scalpel, and none of the laser patients in one trial needed analgesics or experienced bleeding. The CO2 laser’s ability to ablate just the desired tissue without harming surrounding areas facilitates faster orthodontic interventions and improved patient experience.
-
Crown Lengthening and Restorative Access: When more tooth structure needs to be exposed for restorative procedures or prosthetic margins, a CO2 laser can perform soft-tissue crown lengthening with great accuracy. The laser can precisely sculpt the gingiva to the desired height and contour, and if needed, create a trough around the tooth for impression-taking. Because of the laser’s hemostatic action, the working field remains clear, and impressions or scans can often be taken immediately without bleeding interference. Clinical reviews note that lasers provide excellent surgical control in crown lengthening and similar perio-plastic surgeries, yielding optimal aesthetics with minimal inflammation and no sutures. The fractional mode may further be used to promote healing of the gingival margins post-surgery through photobiomodulation.
-
Excision of Oral Lesions (Biopsy, Fibroma Removal): CO2 lasers are widely used to excise benign oral lesions such as fibromas, mucoceles, papillomas, and epulis fissuratum. The laser excises and coagulates simultaneously, often eliminating the need for suturing small biopsies. Importantly, evidence indicates that laser excision can lead to fewer postoperative complications and lower recurrence rates for certain lesions. For example, in the case of oral mucoceles, CO2 laser ablation resulted in no relapses or complications over a 12-month follow-up, whereas conventional scalpel removal had an ~9% recurrence and 13% complication rate (e.g. scar formation). The predictable healing and minimal scarring from laser surgery make it ideal for biopsy sites in visible areas as well. Additionally, the sealed wound reduces pain and often allows patients to resume normal function sooner than with traditional excisions.
-
Periodontal Therapy and Peri-Implantitis: In periodontics, fractional CO2 lasers have emerged as an adjunct for managing periodontal pockets and peri-implantitis. CO2 laser energy can be used in a defocused or fractional manner to decontaminate pocket epithelium and kill bacteria after mechanical debridement. Lasers can access and disinfect deeper pockets more effectively than some mechanical tools, and their use has been associated with reduced postoperative probing depths and inflammation in some studies. The laser’s light energy may also bio-stimulate tissues, potentially enhancing periodontal regeneration. Moreover, for peri-implantitis, CO2 lasers can debride granulomatous tissue around implants and sterilize implant surfaces without physical contact. Clinical reports suggest that high-intensity lasers (including CO2) show promising outcomes in reducing peri-implant inflammation and aiding in re-osseointegration when combined with conventional therapy. While further long-term research is needed, the ability of the DioLaz CO2 laser to switch to a fractional low-power mode is advantageous for gently treating periodontal tissues with minimal invasiveness.
-
Aesthetic Procedures (Depigmentation and Recontouring): Fractional CO2 lasers shine in cosmetic dental procedures aimed at improving smile aesthetics. A common example is gingival depigmentation – removal of melanin hyperpigmentation in patients with “black gums” or uneven gum coloring. Traditional methods like scalpel scraping or bur abrasion can be painful and bloody. In contrast, the CO2 laser can ablate the pigmented epithelial layer in a controlled, layer-by-layer fashion with almost no bleeding and minimal patient discomfort. Clinical studies have reported that CO2 laser depigmentation is safe, effective, and well-tolerated, with most patients experiencing only mild or no pain and achieving complete gingival healing within one week. The laser technique is also relatively fast and can treat the entire aesthetic zone in one visit. Beyond depigmentation, fractional CO2 lasers can perform gingival recontouring for smile design, correction of gingival zenith levels, and even assist in removal of gingival tattoos or aberrant blood vessels. Some practitioners have extended the use of fractional CO2 lasers to non-invasive snoring treatments (by tightening soft palate tissues) and facial skin resurfacing procedures, capitalizing on the same collagen-renewal effects used in dermatology. This broad utility underscores how a system like DioLaz – with both fractional and surgical capabilities – can expand a dental office’s treatment offerings (e.g. minor dermatological aesthetic treatments performed by dentists with appropriate training).
Evidence-Based Advantages and Outcomes
Extensive research and clinical experience support the advantages of CO2 laser techniques over conventional methods across these applications. A 2025 review summarized that laser surgeries (including CO2) in dentistry result in superior clinical outcomes in terms of patient pain levels, operative bleeding, postoperative recovery, and overall satisfaction. Key findings from the literature include:
-
Reduced Intraoperative Bleeding: Virtually all comparative studies note the dramatic reduction of bleeding with laser incisions. One systematic review on frenectomies found bleeding was significantly lower with laser, often described as a dry or bloodless field, whereas scalpel surgery routinely involved more bleeding. The excellent hemostasis improves visibility and may reduce operative time since the clinician spends less time on hemorrhage control.
-
No Need for Sutures: Lasers can often eliminate the need for suturing wounds. Multiple studies report 0% of laser-treated sites required sutures, in contrast to scalpel sites which typically required suturing in 100% of cases. Suture-free healing not only simplifies the procedure, but also spares the patient a second visit for suture removal and reduces foreign-body inflammation in the wound.
-
Less Postoperative Pain and Swelling: By sealing nerve endings and microvasculature, CO2 lasers provoke a milder inflammatory response. Clinical trials of laser vs scalpel consistently show lower pain scores in the laser groups in the hours and days following surgery. For example, in laser gingivectomy and frenectomy patients, pain on the first day is often significantly less than with scalpel, and some laser patients require no analgesics at all. Postoperative edema is also typically reduced, leading to quicker return to normal function (speaking, chewing, etc.). One clinical report described CO2 laser excisions as “painless and with no postoperative swelling,” highlighting the atraumatic nature of laser surgery.
-
Faster Healing and High Patient Satisfaction: Despite some differences in healing patterns (laser wounds may heal by secondary intention under a protective coagulum), the end result is comparable or even better than scalpel healing in many cases. Patients often experience faster functional recovery – able to resume eating, speaking, or other activities sooner. Many also report the healing process to be more comfortable. Studies that surveyed patients who had experienced both laser and conventional procedures found a strong preference for the laser treatment, with significantly higher satisfaction scores for the laser due to the easier recovery. In cosmetic outcomes, lasers have shown long-term success (e.g. depigmented gums remained light in color with minimal relapse many months post-treatment).
-
Safety and Predictability: Modern fractional CO2 lasers are very safe when used with proper settings and precautions (like protective eyewear and controlled airflow). The laser’s shallow penetration (approximately 0.1–0.2 mm effective depth for soft tissue) confines the effect to the target area. This precision, combined with the evidence of lowered complication rates (e.g. fewer infections or scarring), makes laser procedures highly predictable for clinicians. For potentially malignant lesions, CO2 lasers allow complete excision with clean margins and may reduce the risk of seeding abnormal cells, thus potentially minimizing malignant transformation. Overall, the body of research supports that incorporating a CO2 laser like DioLaz can enhance clinical outcomes while maintaining safety.
Connecting DioLaz Features to Clinical Needs: The DioLaz Fractional CO2 Laser has been designed to leverage these advantages in everyday dental practice. Its surgical mode provides a focused beam for precise cutting in surgeries such as gingivectomies, frenectomies, or lesion excisions – fulfilling the clinician’s need for accuracy and control. Meanwhile, the fractional mode delivers an array of microscopic laser spots, useful for therapies like superficial ablation (depigmentation or soft-tissue resurfacing) and biostimulation of tissues to promote healing. This dual capability allows dentists to perform both cutting and regenerative procedures with one device, increasing the scope of treatments available to patients. The high precision of the beam addresses the need to preserve healthy tissue (important in periodontal or cosmetic work), and the strong hemostatic action aligns with the goal of achieving a clean operative field and minimal bleeding. Furthermore, by reducing patient discomfort and downtime, the DioLaz CO2 laser helps meet the growing patient demand for less invasive, faster-healing dental procedures. In summary, fractional CO2 laser technology is a powerful adjunct in modern dentistry – one that can elevate the standard of care across surgical, periodontal, and aesthetic treatments.
Conclusion
Fractional CO2 lasers have proven to be a valuable asset in dental practice, offering a versatile platform for numerous soft-tissue procedures. From routine gingival surgeries like gingivectomy, operculectomy, and crown lengthening to specialized applications in lesion removal, periodontal therapy, and cosmetic enhancements, the CO2 laser consistently demonstrates clinical efficacy. The evidence-based benefits – including reduced bleeding, suture-less healing, lower pain, and rapid recovery – translate into a better experience for patients and more efficient workflows for clinicians. As shown in international studies and reviews, laser-treated cases often exhibit fewer complications and equal or superior outcomes compared to conventional techniques. Tools like the DioLaz Fractional CO2 Laser encapsulate these advantages, providing dental practitioners with precision and flexibility through its dual modes. By embracing such laser technology, dentists can perform procedures with greater confidence in the results, knowing they are backed by scientific evidence and improved patient satisfaction. In an era where minimally invasive dentistry is highly valued, fractional CO2 lasers stand out as an evidence-backed modality that meets clinical needs and enhances the quality of dental care.
References
Khalil M. et al. (2025). Effectiveness of laser-assisted gingivectomy compared to surgical methods: a systematic review. Exploratory Medicine, 6:1001325. DOI: 10.37349/emed.2025.1001325
Roudsari M.B. et al. (2023). Evaluation of the Effectiveness of the Carbon Dioxide (CO2) Laser in Minor Oral Surgery: A Systematic Review. J Lasers Med Sci, 14(1): 1–10. PMID: 38028885
Yagüe-García J. et al. (2009). Treatment of oral mucocele: scalpel versus CO2 laser. Med Oral Patol Oral Cir Bucal, 14(9): e469-e474. PMID: 19415059
Tran T.H.H. et al. (2022). Carbon dioxide laser–assisted treatment for gingival melanin hyperpigmentation: a clinical study. Dentistry Journal (MDPI), 10(12): 229. DOI: 10.3390/dj10120229
Al Asmari D. & Alenezi A. (2025). Laser Technology in Periodontal Treatment: Benefits, Risks, and Future Directions – A Mini Review. J. Clin. Med., 14(6): 1962. DOI: 10.3390/jcm14061962

Share:
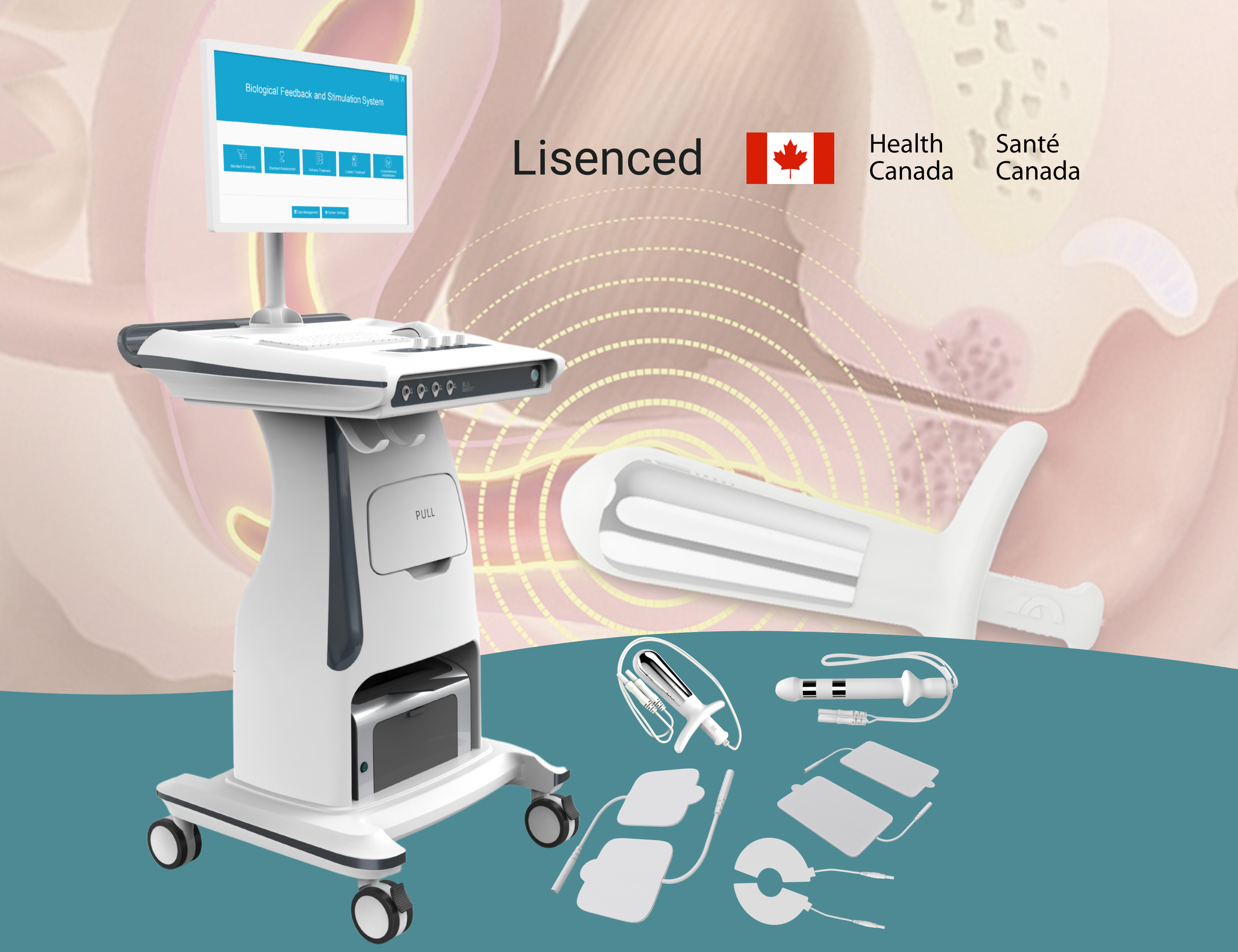
Postpartum Care Combined with Pelvic Floor Device Prevents Pelvic Dysfunction
CO2 Laser Frenectomy for Lip and Tongue Ties: Clinical Outcomes and Advantages