Introduction: Menopause is a natural transition that often brings unwelcome changes to a woman’s pelvic health. Lower estrogen levels and aging tissues can weaken the pelvic floor, leading to problems like urinary incontinence and pelvic organ prolapse. Many postmenopausal women find themselves rushing to the bathroom frequently or noticing discomfort from a slight bladder or uterine prolapse. The good news is that pelvic floor rehabilitation – now enhanced by modern women’s wellness technology – can significantly improve these issues, helping women in menopause regain control and confidence.
Challenges After Menopause
In menopause, connective tissues lose elasticity and muscles may atrophy, meaning the pelvic floor doesn’t support the bladder and uterus as firmly as before. This can result in stress incontinence (leaks during coughs or exercise) or even pelvic organ prolapse (when pelvic organs shift downward). Such changes can hinder an active lifestyle. Traditional advice like doing Kegel exercises is sound, but many women aren’t sure if they’re doing them correctly or enough. Without feedback, it’s hard to strengthen muscles that you can’t see. That’s why a guided pelvic floor rehabilitation program using biofeedback is so beneficial for menopausal women.
Technology-Enhanced Pelvic Rehabilitation
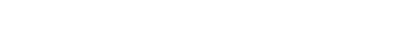
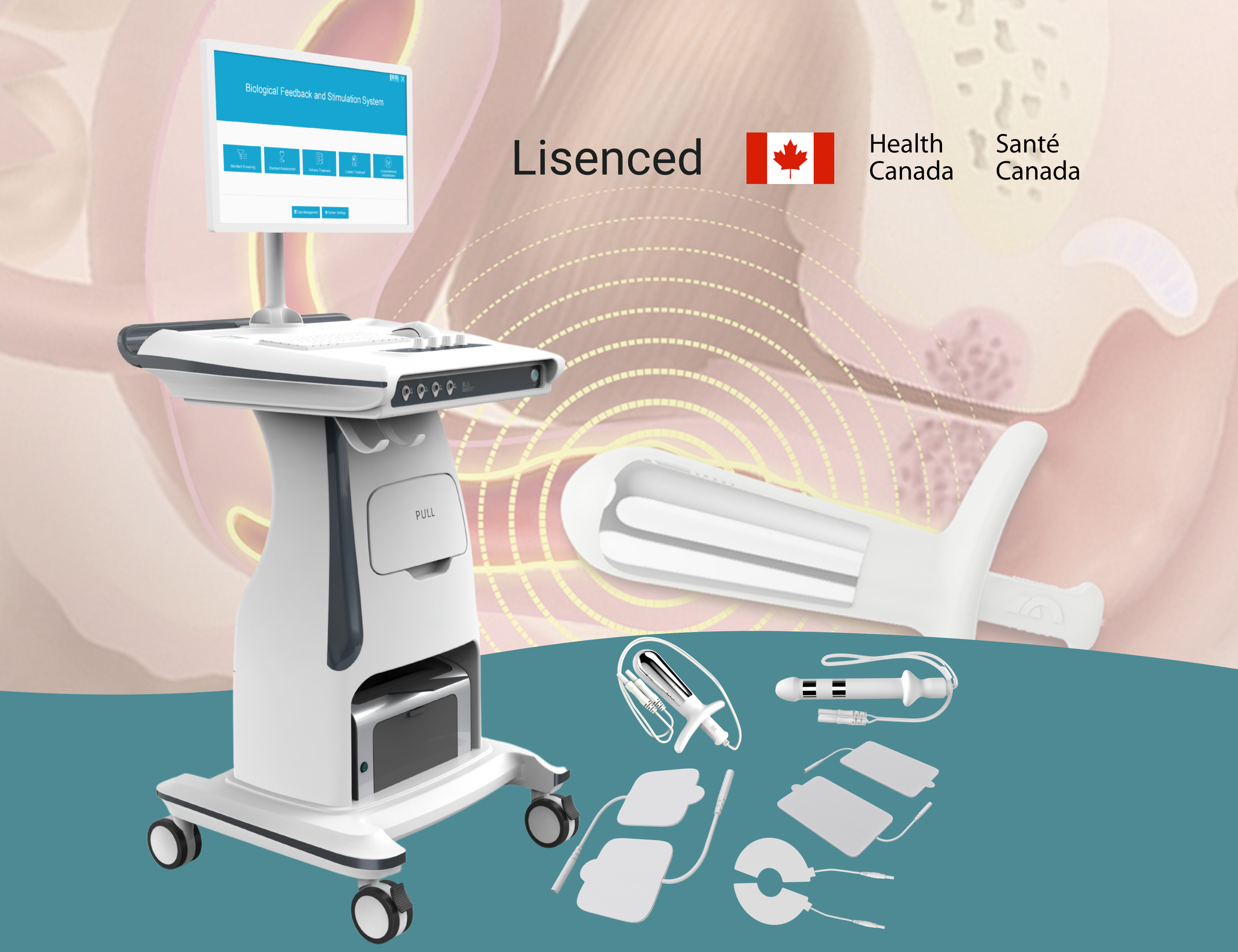
The Medlander B4Plus Biological Feedback and Stimulation System is an example of an advanced pelvic therapy device designed for women’s health. It uses surface EMG biofeedback to detect the user’s pelvic muscle contractions and provides electrical stimulation to help activate those muscles. In practice, this means women exercise their pelvic floor with real-time guidance – a screen shows whether they are contracting muscles effectively, and the device can gently stimulate muscles to contract if needed. This approach leads to measurably better outcomes. Clinical research has documented nearly 95% effectiveness in improving urinary incontinence using biofeedback-stimulation therapy, compared to about 86% with standard pelvic exercise alone. Another study of postmenopausal women with mild pelvic organ prolapse found that after one year of pelvic floor training with biofeedback, 96.7% had their prolapse effectively resolved, vastly outperforming typical results from self-directed exercises. These improvements in continence and organ support demonstrate how technology-assisted rehab can reverse some effects of menopause.
Renewed Confidence and Quality of Life
By strengthening the pelvic floor in a targeted way, women in their 50s, 60s, and beyond can regain freedom in daily life. They can laugh, sneeze, or exercise without fear of leakage and avoid the discomfort of prolapse symptoms. The biofeedback device also tracks progress, which motivates users and their healthcare providers by showing tangible improvements over time. Importantly, addressing incontinence and prolapse has a ripple effect on overall wellness – women sleep better, stay active, and feel more confident socially. Menopause may be a new chapter of life, but with modern pelvic therapy technology, it can be a vibrant and empowered chapter rather than one defined by pelvic health limitations.
References:
- Zhao J. (2023). Biofeedback vs. standard care for urinary incontinence – 94.90% continence improvement with biofeedback-stimulation therapy vs 86.62% with conventional exercises.
- Li Xiqian (2024). Pelvic floor training outcomes in prolapse – 96.67% prolapse disappearance rate after 1 year of biofeedback-based pelvic floor rehab.


Share:
How CO2 Laser Stimulates Collagen and Improves Skin Texture
Understanding Fitzpatrick Skin Types and Laser Energy Settings